Trochanteric bursitis
Greater trochanteric bursitis (GTB) is a very common cause of hip pain. It is a complex pathology and should be thought of as far more than simple ‘bursitis’. So much so that this condition is more commonly referred to as “Trochanteric bursal syndrome” and the intricacies of this pathology could fill a text book.
A bursa is a closed synovial fluid-filled sac that functions as a gliding surface to reduce friction between tissues of the body. The major bursae (plural….and there are over 150 in the body) are located adjacent to joints such as the shoulders, elbows, hips, and knees. The suffix “-itis” infers ‘inflammation’ – tendonitis, meningitis, fasciitis, bursitis etc.
Most commonly bursitis is a non-infectious condition (aseptic bursitis) caused by inflammation resulting from a local soft tissue trauma or repeated irritation. On rare occasions, bursae can become infected (usually a bacterial infection). This condition is called septic bursitis and will not be addressed in this article. Other bursopathies (eg psoriatic, rheumatic or gouty bursitis) are far less common and, like septic bursitis, are best managed medically and not by physiotherapists.
There are several bursae around the hip. By far the most common bursa involved is the ‘greater trochanteric bursa’. Other bursal sources of pain include: the iliopsoas bursa, the ischial bursa (ischiogluteal bursa), the deep trochanteric bursa, the iliopectineal bursa and the gluteus medius bursa. These will not be discussed in this article.
|
Pain from the hip joint (the ball-and-socket) usually presents as pain in the inguinal (groin) region. |
The symptoms of trochanteric bursitis?
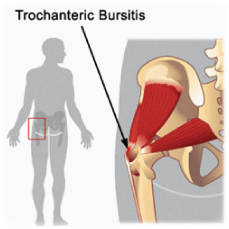 GTB is almost exclusively seen in women between the ages of 40 to 65. It is more common in mothers who have experienced vaginal deliveries. The trochanteric bursa is located on the side of the hip (see opposite). Anatomically, it is separated significantly (5 to 7cm) from the hip joint by soft tissue and bone. When inflamed it can cause considerable tenderness around the bony prominence on the side of the hip and cause pain to radiate along the outer side of the thigh and to the knee. Frequently patients will also experience pain in the gluteal region, sacroiliac region and lower lumbar spine. This can be an indicator of other underlying or causative pathologies that need to be addressed concurrently.
GTB is almost exclusively seen in women between the ages of 40 to 65. It is more common in mothers who have experienced vaginal deliveries. The trochanteric bursa is located on the side of the hip (see opposite). Anatomically, it is separated significantly (5 to 7cm) from the hip joint by soft tissue and bone. When inflamed it can cause considerable tenderness around the bony prominence on the side of the hip and cause pain to radiate along the outer side of the thigh and to the knee. Frequently patients will also experience pain in the gluteal region, sacroiliac region and lower lumbar spine. This can be an indicator of other underlying or causative pathologies that need to be addressed concurrently.
Pain may be exacerbated by side-lying, prolonged walking or stair climbing. Herein lies the difficulty of diagnosing trochanteric bursitis and the challenge to effectively manage the many other pathologies that frequently co-exist. These include: hip arthritis, sacroiliac joint dysfunction, piriformis syndrome, ankylosing spondylitis, gluteus medius or minimus tendonoses…the list is extensive.
How is trochanteric bursitis treated?
Aseptic GTB can be treated very successfully by a skilled physiotherapist. But there are a few points to consider:
- GTB is most easily treated when diagnosed early. Pain that has persisted for more than 3 months will require the co-ordinated efforts of both physiotherapist and doctor. Neither alone are likely to remedy the problem.
- The overwhelming majority of long standing GTB sufferers will have chronic, low-grade lumbar pathology. Management MUST include appropriate treatment of the lumbar spine and/or sacroiliac joints.
- GTB may co-exist with medial gluteal tendonoses or cluneal nerve entrapment – this must be treated concomitantly.
- Consider prolotherapy treatments when insertional gluteal tendonopathy is present or when all other treatments have failed.
- Patients usually have ‘pelvic obesity’ (excessive fat around the bottom/hip/thigh region). This makes manual interventions difficult.
WEIGHT LOSS IS ESSENTIAL.
THIS ALONE WILL OFTEN RESOLVE TROCHANTERIC BURSITIS.
IT WILL ALSO MAKE MANUAL AND INVASIVE MEDICAL INTERVENTIONS FAR MORE SUCCESSFUL AND AFFORDABLE.
|
Patients often state that they are unable to lose weight because pain limits their ability to exercise. Weight loss is a dietary issue and pain (of any sort) should never be used as an excuse for obesity. |
|
Electrotherapy treatments such as ultrasound, TENS, laser or interferential have no place in the arsenal of a skilled physiotherapist and have no proven benefit. |
Physiotherapy treatment
All physiotherapy interventions achieve best results when combined with appropriate medical interventions. To rely on either approach in isolation will seldom result in success.
- Treatment of the lumbar spine or sacroiliac joint – mobilisations, manipulation, mobility and strengthening exercises.
- Release of the gluteal musculature (including gluteal stretches).
- Taping and bracing.
- Gluteus medius restrengthening (poor compliance).
- Posture/ergonomic assessment.
- Orthotic prescription – NOTE – orthotics are usually NOT required to treat this condition but in cases of significant mid-foot pronation with internal tibial rotation during mid-stance, they may provide a modest benefit.
|
Be wary of the practitioner who prescribes orthotics EARLY in the management process. |
Medical treatment
All medical interventions achieve best results when combined with manual treatments – release of the gluteal musculature, lumbar or sacroiliac joint treatments and management of co-existing hip, groin or pelvic pathologies.
- Non-steroidal antinflammatories (oral).
- Steroidal antinflammatories (oral).
- Steroid (cortisone) injections – best performed with medial gluteal tendon steroid injections and gluteal release (physiotherapy).
- Local anaesthetic injections into the TFL, piriformis, and gluteus maximus muscle (best used in combination with stretching and manual release of these muscles).
- Lumbar facet joint steroid injections, root-sleeve steroid injections or steroid epidurals may help to assist the underlying lumbosacral pathology that produces gluteal tightness and perpetuates irritation of the trochanteric bursa.
Prolotherapy treatment
Extracorporeal shockwave therapy is an extremely effective treatment for GTB. It is as close to a ‘magic bullet’ as it gets. It is especially useful in cases where lateral gluteus medius or minimus tendonopathy co-exists. However it is not a first-line treatment for several reasons:
- It is uncomfortable for the patient. Each treatment takes around 5 minutes and it leaves most patients feeling ‘bruised’.
- Usually 6 treatments are required (1 or 2 treatments per week) and often a ‘recovery’ period between treatments 4 and 5 is necessary – 2 weeks of rest.
- Full results occur around 8 weeks after the last treatment. In other words, shockwave therapy is a reliable form of treatment but it is NOT a quick-fix.
Kingsley Medical offers a course of 6 shockwave treatments for $300. If additional treatments are required to achieve full resolution, these are provided free of charge.
Platelet rich plasma or sclerosing agents are also beneficial to treat bursitis and must be performed under ultrasound guidance. These options are also available through Kingsley Medical.
Surgical treatment
Surgical excision of the bursa (bursectomy) is rarely performed in isolation but may be performed during hip joint replacement surgery. However unless the underlying biomechanical stressors are addressed the bursa may ‘re-form’ and become symptomatic.
Surgical reattachment of the gluteus medius or minimus tendons (if ruptured) can assist with hip and pelvic stability and reduce the work-load of gluteus maximus – this reduces irritation of the trochanteric bursa. Intense retraining of the gluteus medius or minimus muscles is required post-operatively and needs to be progressed with caution by an experienced therapist.
Lumbar facet rhizotomies or sacroiliac rhizotomies (percutaneous rhizotomy or neutomy) can be extremely helpful to assist with the treatment of GTB. The involvement of the lumbar facet joints or sacroiliac joints needs to be assessed by an experienced physiotherapist or musculoskeletal doctor as radiographic imaging is often misleading or uninformative.
In cases where severe lumbar pathology contributes to the presentation surgery may be required in the form of either micro-discectomy, laminectomy or segmental fusion.
|
Take home message |
- Trochanteric bursal syndrome is a complex problem that is frequently misdiagnosed and mismanaged.
- Treatment must address lumbar and pelvic issues that co-exist.
- A single steroid injection into the bursa seldom provides permanent relief. A second injection given as soon as ANY pain returns can be sufficient to give permanent results. This may be required in as little as one to two weeks after the first injection. Repeated steroid injections are often avoided by physicians but in this instance they are safe and can prove extremely beneficial.
- Prolotherapy such as shockwave therapy or platelet rich plasma are very effective treatments for chronic cases of GTB.
- Physiotherapy treatment is most effective when coordinated with medical interventions.
If you have any further questions on this subject, or you would like to contact the physiotherapist best suited to managing your problem please call or email us.