Plantar fasciitis/ heel spurs
What is plantar fasciitis?
 The plantar fascia is a strong band of connective tissue that supports the arch/soul of the foot. It provides some structural integrity to the small bones of the foot and assists with propulsion of the foot when walking. Plantar fasciitis (inflammation of the plantar fascia) is a common condition affecting adults and results in pain at the bottom of the heel. This pain can extend further to include the side of the heel and the arch of the foot. It is more commonly seen in women and frequently found in overweight individuals. Pregnant women, runners and workers who spend long periods on their feet are also susceptible to plantar fasciitis.
The plantar fascia is a strong band of connective tissue that supports the arch/soul of the foot. It provides some structural integrity to the small bones of the foot and assists with propulsion of the foot when walking. Plantar fasciitis (inflammation of the plantar fascia) is a common condition affecting adults and results in pain at the bottom of the heel. This pain can extend further to include the side of the heel and the arch of the foot. It is more commonly seen in women and frequently found in overweight individuals. Pregnant women, runners and workers who spend long periods on their feet are also susceptible to plantar fasciitis.
What are the symptoms?
The pain of plantar fasciitis is typically most severe first thing in the morning or upon standing after sitting for a period of time. These first few steps can be extremely painful though often this pain will subside after several minutes of walking. People may get relief from the pain of plantar fasciitis by changing the shoes they wear or by minimising their walking and running. Additionally, some people will get relief by soaking their foot in warm water or massaging the heel of their foot (using their knuckles or even a golf ball).
Plantar fasciitis and heel-spurs
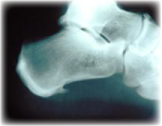 Often patients with plantar fasciitis will be told that they have ‘heel spurs’ (pictured opposite). This is a little misleading as it implies that the bony spur that sometimes forms at the bottom of the heel is responsible for their pain. Many people have spurs on their heel without having any pain at all. Likewise many people have considerable heel pain without any x-ray evidence of a bony spur. The medical and physiotherapy management of plantar fasciitis is not affected by the presence or absence of a spur and hence x-rays are usually not warranted.
Often patients with plantar fasciitis will be told that they have ‘heel spurs’ (pictured opposite). This is a little misleading as it implies that the bony spur that sometimes forms at the bottom of the heel is responsible for their pain. Many people have spurs on their heel without having any pain at all. Likewise many people have considerable heel pain without any x-ray evidence of a bony spur. The medical and physiotherapy management of plantar fasciitis is not affected by the presence or absence of a spur and hence x-rays are usually not warranted.
Physiotherapy assessment and treatment of plantar fasciitis
Patients with plantar fasciitis will be assessed by their physiotherapist for the likely cause of their pain – poor footwear, altered foot biomechanics, weight gain etc. In patients that present with heel pain (especially children) the physiotherapist must exclude other possible diagnoses such as Severs condition, Achilles tendonitis, septic arthritis, reactive arthritis, osteomyelitis and juvenile arthritis. The physiotherapist will assess the patient’s foot biomechanics to determine if orthotics (inserts that are worn inside the shoe) are necessary. Most footwear can accommodate an orthotic so being told that you need to wear orthotics does not condemn you to a life of unfashionable footwear.
 You will then be shown how to stretch your calf muscles as well as the plantar fascia itself. You will need to continue with this regularly each day for at least 1 to 2 weeks as the pain resolves. Ideally, someone you trust (and love dearly) can be shown how to massage your calves and your plantar fascia at home. This regular massage (as simple as it is) can make the world of difference in the recovery time and can SIGNIFICANTLY reduce your physiotherapy costs. Many patients will massage the heel of their foot using a golf ball. It is not a comfortable remedy but the pain of doing it will usually settle within 4 or 5 minutes and, when done each day, this can drastically reduce the recovery time.
You will then be shown how to stretch your calf muscles as well as the plantar fascia itself. You will need to continue with this regularly each day for at least 1 to 2 weeks as the pain resolves. Ideally, someone you trust (and love dearly) can be shown how to massage your calves and your plantar fascia at home. This regular massage (as simple as it is) can make the world of difference in the recovery time and can SIGNIFICANTLY reduce your physiotherapy costs. Many patients will massage the heel of their foot using a golf ball. It is not a comfortable remedy but the pain of doing it will usually settle within 4 or 5 minutes and, when done each day, this can drastically reduce the recovery time.
Your physiotherapist may also decide to tape your foot – this is ideal in patients who cannot wear orthotics (or whilst their orthotics are being made) and in patients who have only mild biomechanical dysfunction of the foot. Again, someone can readily be taught how to apply this taping (or you can learn to do it to yourself) and this will reduce the amount of physiotherapy you require.
Treating stubborn plantar fasciitis
Physiotherapy should resolve the pain of plantar fasciitis within 10 to 14 days. If progress is slow you may be asked to trial a short course of non-steroidal anti-inflammatories whilst you continue with home treatment (stretches, taping, massage etc). Additionally you may be instructed to wear a ‘night splint’ (pictured opposite) – a device that stretches your calf overnight (or for several hours at a time). This is usually used for 1 or 2 weeks and can be very effective in relieving stubborn cases of plantar fasciitis.
 In particularly difficult cases (when pain has persisted for more than 6 months) or in situations where symptoms return, patients may be encouraged to have a corticosteroid injection into the heel. This is not a terribly pleasant option and needs to be done by a doctor who is trained in the procedure but it frequently gets very good results. It is important however that you continue with your stretches, taping and massage for at least a further week at home after you have had this injection.
In particularly difficult cases (when pain has persisted for more than 6 months) or in situations where symptoms return, patients may be encouraged to have a corticosteroid injection into the heel. This is not a terribly pleasant option and needs to be done by a doctor who is trained in the procedure but it frequently gets very good results. It is important however that you continue with your stretches, taping and massage for at least a further week at home after you have had this injection.
Your physiotherapist can also discuss the use of extracorporeal shockwave diathermy, prolotherapy or surgery for plantar fasciitis.
If you have any further questions on this subject, or you would like to contact the physiotherapist best suited to managing your problem please call or email us.
© Andrew Thompson