Ankylosing Spondylitis
Ankylosing spondylitis (AS) is a progressive and potentially disabling inflammatory disorder. It primarily affects the sacroiliac joints and the spine (the axial skeleton). AS is a genetic, immune-mediated disease, and is strongly associated with the HLA-B27 genotype.
Epidemiology
Ankylosing spondylitis affects around 0.5% of the population (one in 200 individuals) and is thought to account for as much as 5% of patients presenting with long-standing back pain. It affects more men than women and typically between the ages of 20 and 40 years.
Symptoms
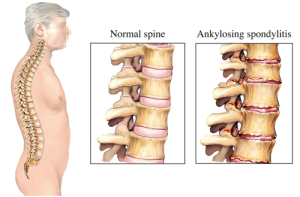 The pain of AS is caused by inflammation of the sacroiliac joint or the facet joints of the spine – sacroilitis and spondylitis. Syndesmophytes (bony growths originating from within ligaments of the spine) lead to ankylosis (bony fusion) of the spine and stiffening
The pain of AS is caused by inflammation of the sacroiliac joint or the facet joints of the spine – sacroilitis and spondylitis. Syndesmophytes (bony growths originating from within ligaments of the spine) lead to ankylosis (bony fusion) of the spine and stiffening
Other symptoms include asymmetric oligoarthritis, and enthesitis, (inflammation of the insertional points of ligaments, tendons and joint capsules at the bony attachment site). Enthesitis often presents as Achilles pain, plantar fascioses or chest wall pain.
Ankylosing spondylitis is also associated with a number of extra-articular manifestations – ‘non-joint’ related problems.
- Ocular: Acute anterior uveitis is a common associated symptom of ankylosing spondylitis. It typically presents as an acutely painful red eye with blurred vision and photophobia.
- Gastrointestinal: Approximately 60% of AS patients have mucosal inflammation on colonoscopy, with symptomatic inflammatory bowel disease occurring in 10% of patients.
- Skin: Psoriasis has been identified in up to 20% of patients with AS.
- Bone: Osteopenia and osteoporosis are common occurrences, with the risk of vertebral fracture approximately seven times that of the general population.
- Cardiac: Conduction disturbances and aortic incompetence are in higher in AS sufferers.
- Pulmonary: Pulmonary abnormalities such as airway disease, apical pulmonary fibrosis and pleural thickening are also more prevalent in AS patients.
- Renal: There is an increase in renal abnormalities and functional loss in AS patients.
Diagnosis
 AS is diagnosed by both clinical presentation (symptoms) and radiographic imaging. It is important to note that many inflammatory arthropathies may not show any radiographic change in early presentations. Diagnosis includes a combination of: limited motion of the spine, persistent lower back pain (lasting more than 3-months), limited chest expansion and radiographic evidence of sacroilitis.
AS is diagnosed by both clinical presentation (symptoms) and radiographic imaging. It is important to note that many inflammatory arthropathies may not show any radiographic change in early presentations. Diagnosis includes a combination of: limited motion of the spine, persistent lower back pain (lasting more than 3-months), limited chest expansion and radiographic evidence of sacroilitis.
Assessment
Assessment should include a thorough history in order to differentiate mechanical from inflammatory back pain. Inflammatory back pain may be suspected in patients with fatigue, morning stiffness and pain that is not relieved by rest. Additional symptoms of systemic tendon pain, ethesopathic pain or tenderness and shortness of breath with exertion may lead the clinician to suspect AS.
Management
Non-pharmacological management
It is vital to educate the patient on the progression of the disease, the importance of exercise and the maintenance of posture. It is also essential to maintain fitness and cardiac function.
Physiotherapists are integral in maintaining both fitness and flexibility in their patients. In the early stage of the disease, land or gym-based cardiovascular exercises are important. This may progress to hydrotherapy if pain is severe or joint function inhibits land-based exercise. Motivation (for ANY patient) is difficult and a good therapist will need to be dynamic and enthusiastic to achieve results.
Medical management
Non-steroidal antinflamatory drugs (NSAIDs) are considered the first-line drug treatment for AS patients.
Anti TNF-α therapy: This class of medications has been shown to be very effective in the treatment of AS and is second-line treatment in patients who have been non-responsive or intolerant of NSAIDs .
These medications must be initiated by a rheumatologist as they are costly to Medicare and may pose significant complications – primarily an increased risk of infection. These classes of medication has been shown to both increase susceptibility to tuberculosis (TB) and reactivate latent TB. (It is mandatory to screen for TB prior to commencing treatment with anti-TNF medications).
Anti TNF-α therapy is associated with an increased risk of melanoma and other skin cancers so regular skin checks with a suitably qualified GP or dermatologist is essential – more so in cases where there is a familial predisposition to developing skin cancers.
Summary
Key features of Ankylosing Spondylitis:
- Back pain or stiffness with gradual onset – weeks or months.
- Early morning pain or stiffness that reduces with movement.
- Pain or stiffness that improves after exercise and is worse after rest.
- Sleep disturbance, particularly during the second half of the night.
- Persistence of the above symptoms for more than three months.
- Pain that is relieved temporarily after a shower, bath or heat treatments.
- Inflammation of the iris within the eye, which may include pain in the eye or brow region, pain associated with exposure to light, blurred vision or a reddened eye.
- Symptoms which began in late teens or 20s.
Take home message for patients:
- Stay fit.
- Cease smoking.
- Improve/maintain flexibility /of the spine.
- Physiotherapy to maintain joint mobility and posture.
- Regular contact with your GP to monitor side effects of medication, to treat infections early and discuss alternate treatment options if adverse reactions are an issue or pain persists.
- Early consultation with a rheumatologist to initiate treatment with anti-TNF-α therapy if NSAIDs are ineffective.
© Dr Andrew Thompson